A telemedicina é uma realidade
A pandemia causada pelo novo coronavírus trouxe inúmeros desafios para a área da saúde. Entre eles, manter o acompanhamento de pessoas em tratamento de saúde de forma segura.
A solução implantada no Hospital Universitário da UFSC, utilizando tecnologia desenvolvida na universidade, é a Telepediatria, que permite atendimento a distância aos usuários do SUS.

Segundo Aldo von Wangenheim, Prof. Dr. rer.nat. at UFSC, “A continuidade, com segurança, da oferta de serviços de atendimento pediátrico durante a pandemia é essencial. É especialmente importante oferecer ao pediatra ferramentas para o atendimento continuado de crianças já em tratamento, ao mesmo tempo oferecendo a segurança do paciente poder ser atendido em casa e de se poder abrir um bom canal de comunicação com os pais. O Serviço de Pediatria do Hospital Universitário da UFSC, junto com o Núcleo de Telessaúde de Santa Catarina e o Sistema Integrado de Telemedicina e Telessaúde – STT, implantou um serviço de Telepediatria, aproveitando a abertura dada pela nova Lei da Teleconsulta e a infraestrutura de cobertura em 5 estados oferecida pelo STT. Neste artigo, recém publicado no mais conceituado periódico internacional de Telemedicina, relatamos os primeiros resultados obtidos“
Teleconsultations at a Pediatrics Outpatient Service in COVID-19 Pandemic: First Results
Camila Marques de Valois Lanzarin, Aldo von Wangenheim, Thaïs Cristina Rejane-Heim, Fernanda de Souza Nascimento, Harley Miguel Wagner, Heloisa Silva Abel, José Djalma da Silva Júnior, and João Carlos Xikota
Abstract
Objective: Describe our experiences using teleconsultation approach to care for pediatric subspecialty follow-up patients during pandemic period.
Methods: Synchronous teleconsultation solution was developed and implemented as a multiplatform/multimodality service, capable or running on desktop browsers and smartphones, and capable to handle chat, audio, and video. Term of consent was applied. Absolute number and percentage of patients assisted, as well as the form of consultation and the mean of attendance per patient were presented.
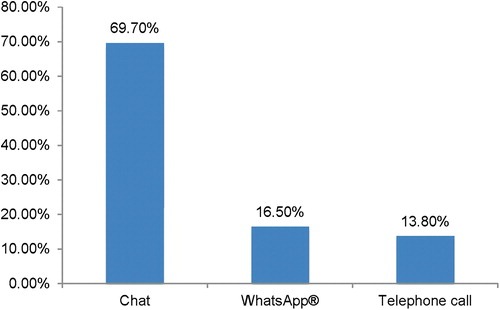
Results: A telemedicine service was started using tools provided by The Santa Catarina State Integrated Telemedicine and Telehealth System offering real-time chat, through an online-based teleconsultation service. We assisted 75 patients in 109 consultations in 3 months, of which 69.7% were performed by chat. Mean of consultations per patient was 1.45.
Conclusion: To our knowledge this is the first service in offering this modality of medicine for Brazilian public health care system. Patients and health care personnel reported satisfaction.
Background
State of Santa Catarina (SC) is located in the south of Brazil, with an estimated population of 7,164,788 inhabitants.1 The State, in partnership with Federal University of Santa Catarina (UFSC), has developed a large-scale asynchronous telemedicine network, which has been in place for the past 15 years. SC State Integrated Telemedicine and Telehealth System (STT/SC) offers coverage to 100% of the municipalities, integrates primary, secondary, and tertiary health care facilities in a single infrastructure,2–6 and has been responsible for >9.5 million tele-examinations and >120,000 inter-consulting between primary health care staff and specialists. Specific modules for many specialties are available, such as teleradiology,7 telecardiology,8 and teledermatology.9 Tests with a telepathology module are also in progress.10 STT/SC was always oriented exclusively toward asynchronous services: As part of the SC State public health care infrastructure, two of the requirements of the service were (1) to optimize the scarce resources represented by medical specialists and (2) to maximize access to specialized medical services to all patients. Real-time telemedicine is time-consuming, especially for the specialist, who has to be present at a consultation or examination instead of providing an expert opinion or a findings report. This strongly limits the amount of patients, examinations and primary health care staff questions a single specialist can take care of. In these 15 years of operation we have systematically been implementing a strongly asynchronous service-oriented policy. We interpreted the continuous success and growing of the STT/SC as a confirmation that our policy was correct. Coronavirus disease 2019 (COVID-19) crisis changed everything: suddenly, synchronous teleconsultation services were acutely needed.
Teleconsultation was exceptionally approved by the Brazilian Federal Council of Medicine for the COVID-19 pandemic period, allowing the practice of medicine by synchronous methodologies with the objective of direct health assistance between physician and patient.11 The Brazilian government also authorized telemedicine service under Law 13,989/2020.
Public health care system in SC concentrates all pediatric specialties at tertiary and quaternary medical services in large population centers, similarly to other locations.11–13 As a consequence, patients from all over the state, sometimes from locations hundreds of miles away, are referred to our institution, a tertiary center for pediatric care. Use of telemedicine in pediatric care was not yet carried out in our state, even though synchronous telemedicine has been described to be an excellent alternative to overcome the travel and time barriers that arise when long distances or transportation difficulties separate patients from pediatric subspecialty.13
In view of social distancing and a restriction of elective consultations decreed by the state government on March 17, 2020, medical care at our outpatient pediatric reference center was reformulated. This article describes our first experiences in using a teleconsultation approach with pediatric subspecialty follow-up patients during the pandemic period.
Methods
From a technological point of view, to be able to publish a synchronous teleconsultation solution in the shortest span of time, with minimum costs and that could be seamlessly integrated as a module into the STT/SC, we implemented our teleconsultation application as a multiplatform/multimodality service, capable or running on desktop browsers and smartphones, and capable to handle chat, audioconference, and videoconference. For this purpose, we are continuously developing and improving a reactive web application14 that behaves similar to a webpage on a desktop browser and has the look-and-feel of an app when running on a smartphone. This allowed us to follow a fast single-code/no-installation-needed philosophy: Each new version is deployed only once on the STT/SC server and all users automatically download this version when they use the app the next time. We followed a rapid versioning process, where we started with a simple version, to launch the service as soon as possible, and have been incrementally refining it and adding functionality since.
From a service point of view, the use of telemedicine was approved by the institution’s medical board, through the process (IRB) SEI number 23820.003562/2020-17. To be able to start providing the teleconsultation, we first reviewed medical report of our patients to determine the eligible cases for online medical care. In addition, priority was given to patients who contacted us requesting online care. All selected cases were guided through a phone call to assist them in how to use the app and to schedule the first appointment. When family did not have access to internet or could not use the chat, the consultation was performed through a telephone call.
Access to the teleconsultation platform was performed through the hospital website (www2.ebserh.gov.br/web/hu-ufsc) by simultaneous access of the patient and the attending physician. Families access the platform using the number of the patient national individual registration, registered at the Unified Health System. Visit started only after the acceptance of the term of consent, which was carefully composed to offer guidance regarding the importance of providing reliable information using this platform (HIPPA compliance system)—Figure 1.
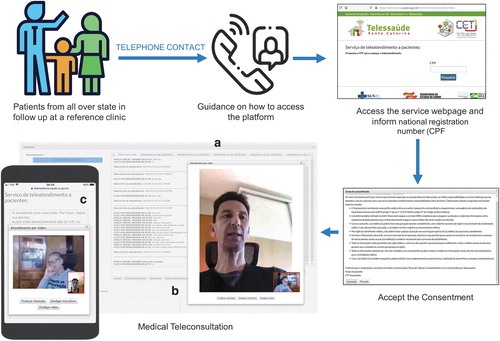
Our online medical care service started with simple chat and the possibility of sending and receiving files from patient and physicians. It has gradually been improved. All data exchange occurs directly between the patient’s family and the physician. All the exchanged information is automatically saved in the patient’s health record at our institution. When necessary, an in-person appointment for a physical examination was scheduled. Patients were also directed to go to primary health care units near their residence when additional information was required, such as anthropometric measurements. These additional data were collected at the next appointment.
In this article, we focus on our experiences and results from April to June 2020, when we offered only the chat and file transfer functionalities of our teleconsultation module. We present the absolute number and percentage of patients assisted of consultations done through chat, the number of patients who could not access the chat, as well as the form of consultation and mean of participation per patient. We qualitatively present the reason for the refusal of chat-based care and we describe our perception using this modality of telemedicine. At this first stage, we did not provide a formal evaluation questionnaire, but rather conducted qualitative feedback interviews with medical staff and patients’ parents. All staff and patients’ families have provided consent for the publication of this material in this study and on the YouTube channel of the SC State Telehealth Centre.
Results
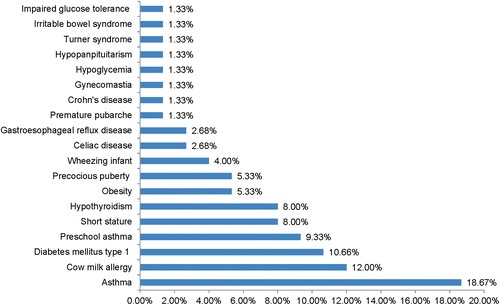
To guarantee the continuity of pediatric care in gastroenterology, endocrinology, and pneumology during the present pandemic context, we deployed a pediatric telemedicine service using a tool provided by the State Telemedicine Network, SST/SC, initially offering real-time chat to patients through an online-based service of teleconsultation. During the 3 months covered by this report, it allowed us to assist patients who needed follow-up care, with various pathologies (Fig. 2). We assisted 75 patients, in 109 consultations, of which 69.7% were performed using our integrated chat module, 16.5% employed the WhatsApp® mobile application, and 13.8% were performed through a telephone call (Fig. 3). Problems with registering in the Unified Health System to access the chat, not having access to the internet, and not being able to understand the guidelines for accessing the chat or not be able to use the chat were the reasons for the use of WhatsApp or a telephone call. Mean of consultation per patient was 1.45. Gastroenterology and endocrinology performed more consultations per patient than pneumology. Children from all over state were assisted.
This teleconsultation service allowed us to maintain this segment of medical assistance with, we understand, similar quality standards during this pandemic context. This allowed us to closely monitor our patients, offering treatment for chronic diseases or pathologies amenable to distant medical follow-up. During this trajectory, we developed new communications skills to ensure optimal information exchange between patients and doctors for a clear interpretation of the patient’s symptoms and questions as well as a correct understanding of the given medical instructions.
Yet, we noted a considerable increase in consultation time and a need for repetitive appointments in some cases, to ensure a complete understanding of the patient regarding all given medical instructions as well as to mitigate the insecurity feeling of the patient after a nonphysical medical consultation. We believe that could be related by the fact that the chat is a written form of communication, different from a common consultation. Our medical team has shown a high degree of satisfaction with the tool; however, future evolution to the audiovisual assistance will be helpful to improve the understanding of medical instructions and to permit the evaluation of some physical examinations signs. We considered that a chat is not a good choice for first consultations, when a doctor–patient relation is not built yet.
Although many patients have shown doubts and are still unaware of this new model of care, most families that used our service report satisfaction and enjoy the new experience. Constant changes have also been made in this new modality, continuously improving the quality of the service offered, enhancing the accuracy of the data analyzed for the health care team. We compiled some of the qualitative feedback interviews with medical staff and patients’ parents in a short documentary, available at http://bit.ly/telepediatrics.
Discussion
The SARS-CoV-2 pandemic has deeply affected every aspect of health care. As in other countries, Brazil is now experiencing a large-scale outbreak, and this situation has motivated fundamental changes in the health care system. In this context, telemedicine has an essential role, expanding health care across the country.15
In Brazil, telemedicine was initially described in 1990 by educational establishments and health research centers.16 In SC, telemedicine was already a consolidated tool before the pandemic COVID-19, used statewide since 2005 in asynchronous mode.2–6 Development and application of a synchronous platform in our state has an essential role in pandemic response, expanding health care. Telemedicine can offer continuous care to chronic patients and ease the panic caused by the global pandemic.15,17
Even if this online-based service showed a broad acceptance, we could identify inherent difficulties in accessing this service modality, either by individual limitations, such as a lack of computer skills, or caused by obstacles imposed by areas with limited internet access. Furthermore, the absence of a physical examination, as well as nuances of the clinical assessment, still pose barriers to teleconsultations.12,18 Other barriers already described in the literature, such as difficulties to use a chat app and difficulties in writing and understanding written orientations, were limitations we could also observe.
Nevertheless, internet-based medical technologies have progressively evolved during the past decades. The possibility of real-time low-cost videoconferences with increasingly high-quality and wider access has expanded the possibilities of online-based health care, whereas recent studies have proved the safety and effectiveness of telemedicine, especially teleconsultations.18–21 We are now starting a second phase of our project, with audiovisual assistance. The main objective will be to allow for a faster and more dynamic communication and overcome patients’ difficulties in writing and understanding written orientations. It should also allow some degree of visual evaluation, aiming at reducing the absence of a physical examination.
In our practice with telemedicine, opposed to Greenhalgh et al.,21 we perceived that there was an increase in the duration of consultations, probably because of the use of the written chat. However, we agree that during the consultation, there is the need to explicit things that were normally implicit during a presential consultation. We also see the importance of a pre-existing relationship of trust between doctor and patient.18,21
Catapan and Calvo18 predicted that the Brazilian public health care system would present significant changes only in response to a growing demand for telemedicine coming from the population. The COVID-19 pandemic crisis changed the slow adoption process of telemedicine the public health care sector was experiencing and provided the necessary incentive to extend the palette of services of the telemedicine system already in operation in our state.
Conclusions
To our knowledge, this is the first service implementing teleconsultation for pediatric patients in the Brazilian public health care context. During the period covered by this report, we provided 109 teleconsultations for 75 patients, 69.7% of which were performed through the integrated platform developed by the STT/SC. We considered the role of teleconsultations and of telemedicine in general of the utmost importance to allow for a geographically independent and agile patient follow-up during the pandemic period.
Authors’ Contributions
All authors fill the criteria of authorship, defined by the International Committee of Medical Journal editors.
Disclosure Statement
This study was performed at the University Hospital at the Federal University of Santa Catarina. The authors declare no conflict of interest regarding the publication of this article.
Funding Information
No funding was received for this article.
Assista também ao vídeo, com entrevistas de médicos e pais, disponível no canal Papo Saúde do Telessaúde SC.
Conheça mais sobre esse serviço neste Papo Saúde!
Fonte: https://doi.org/10.1089/tmj.2020.0471
Ficou curioso sobre o STT? Acesse as nossas páginas em telessaude.sc.gov.br ou telemedicina.ufsc.br ou então contacte-nos em contato@incod.ufsc.br.
UFSC realiza formatura online para a centésima turma do curso de Medicina
UFSC realiza reunião aberta online para esclarecer dúvidas sobre diploma digital
Santa Catarina mapeia o uso de blockchain para transações financeiras